To design multipathogen serosurveillance, it is important to establish the associated use cases (high-level policy-relevant questions), expected outcomes, and target measures for each priority pathogen of interest.
- Home
- Multiplex study design
Table 1. Example description of priority pathogens and the associated policy-relevant questions and target measures to be estimated in a multipathogen serosurvey.
| Pathogen | High-level policy-relevant question | Expected outcome | Target measure |
|---|---|---|---|
| Dengue | Should dengue vaccine be used, and, if so, where and which vaccine should be used? | Identification of areas with endemic transmission | · National seroprevalence · Sub-national age-specific seroprevalence (force of infection – FOI) |
| Typhoid | What is an effective vaccine strategy for the Typhoid Vi-Tetanus Toxoid conjugate Vaccine (TCV)? | Identification of areas with high disease burden | · National seroincidence · Sub-national seroincidence |
| Cholera | Can we augment case-based surveillance data to design targeted strategies for the Oral Cholera Vaccine (OCV)? | Identification of areas with high disease burden | · National seroincidence · Sub-national seroincidence |
| Diphtheria | Is the vaccination coverage of diphtheria sufficient for control or are supplemental immunization activities (SIAs) needed? | Estimation of diphtheria vaccination coverage (≥DPT1) | · National seroprevalence · Division level seroprevalence |
Pathogen selection
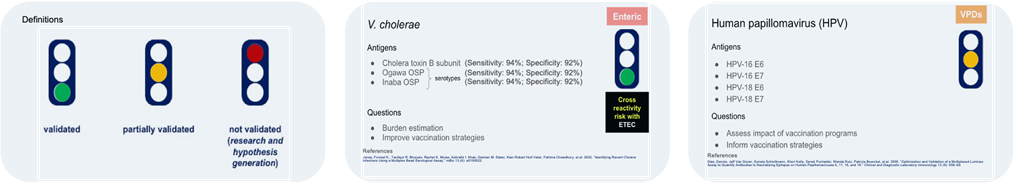
Determining the priority pathogens of interest and the full antigen panel to be tested for using the MBA is a process that should be done with the relevant policy decision-makers in country or administrative unit where serosurveillance is being conducted, as was done in Kenya. Engagement or buy-in from such individuals from the start is important for these data to be useful. To determine which pathogens should be tested, first examine which pathogens have antigen markers that have been validated for determining prior infection and/or vaccination. Using a similar framework as Figure 1, may help identify what questions can currently be answered for different pathogens using this assay platform.
Sampling strategy and survey design
Determining the survey design is a critical aspect of study design and seroepidemiology. This will ultimately affect any inference made and, therefore, requires careful attention. Survey design is directly related to the objectives or use cases, expected outcomes, and target measures of the priority pathogens. Below are some primary considerations for determining your survey design for multipathogen serosurveillance:
- Cross-sectional versus longitudinal serosurveys for surveillance
- Nested study designs within existing surveys like Demographic & Health Surveys (DHS) or Sample Vital Registration Systems (SVRS)
- Residual biorepositories (i.e., leveraging existing serum collected from surveys like DHS or healthcare facility specimens).
- Administrative level for the survey (national versus subnational administrative level)
- Balancing the number of communities/clusters and households to sample to achieve spatial precision
- When to collect data may depend on
- Pathogen-specific use cases (e.g. evaluating burden of disease before and after intervention implementation or during high versus low transmission season) or
- Maximizing enrollment (e.g., during less migratory seasons or waiting after climate disasters like flooding).
- How frequently to survey and sample individuals cross-sectionally or longitudinally in serosurveillance (i.e., to conduct serosurveillance in a population cross-sectionally every 3 years based on how frequently disease patterns or antibody kinetics may change).
- Selection of target populations by demographic characteristics (and/or geographic characteristics) across antigens
- Calculation of sample size to address different use cases for various pathogen-specific antigens (i.e., minimizing the margin of error or precision around the intended target measure estimates like seroprevalence)
- Collection of core individual- and household- survey data to accompany serum data collection (e.g., age, sex, household GPS location)
- Selection of type of specimen to be tested (e.g., dried blood spot versus venous serum) [Specimen Collection Procedures]
FAQs about survey design
These are frequently asked questions about designing serosurveys. There is no single ”correct” answer to these: the decision will depend on the goal of the study and will be influenced by multiple considerations, including those that are outlined below. The JHU Seroanalytics Hub is actively working to develop tools to guide users to make decisions on serosurvey design.
Considerations
- Feasibility: Conducting a cohort study following the same individuals over time is generally more resource-intensive than a serial cross-sectional study that samples different individuals per round.
- One option is to use a nested study design wherein a cross-sectional survey is performed and only a subset of participants are enrolled for longitudinal follow-up. This option is beneficial if there are specific research questions that can only be addressed with longitudinal data (e.g., estimating seroconversion, understanding antibody kinetics or waning immunity of certain infections or vaccines).
- Alternatives such as an adaptive design allow modifications to the study sampling design (i.e., sample frame and/or sample size) to improve statistical inference without compromising validity.
- This approach is largely borrowed from the field of clinical trials and cancer epidemiology.
- The benefits of this type of design are that based on interim analyses, the sampling approach can be reviewed and adapted to conserve resources, including to refine the sample size based on updating refusal rates, changing the enrollment of the same individuals per round to different, or updating when recruitment is conducted to capture the seasonality of certain infections.
- This design approach does have ethical considerations as the master protocol will require amendments. Messaging to the institutional ethical review board should be carefully considered.
- Epidemiologic inference: The selected study design will affect what epidemiologic inference is possible with the generated data.
- In a cohort study, key epidemiologic metrics such as the attack rate (i.e., the proportion of the cohort that seroconverted between two rounds) can be directly measured. However, cohort studies can suffer from loss-to-follow-up and, if this is differential by space, time, or demographics, can bias attack rate estimates.
- In a serial cross-sectional study, the change in seroprevalence between two rounds provides an estimate of the population-level attack rate. However, the samples from the two rounds must be comparable, even if from the same source population.
- Survey weights: There are multiple ways to conduct a serial cross-sectional study. If participants included in one round are not eligible to be included in another round, this will affect the survey weights and statistical inference. If participants are sampled randomly for inclusion at each round (where some individuals may be included in multiple rounds due to chance), then this will not affect the survey weights. Careful thought should be given to how individuals are sampled across rounds.
Considerations
- Study design: The choice of study design is based on whether the same or different individuals will be included each survey round (i.e., cross-sectional, longitudinal, or nested), and what the desired epidemiologic inference is (see Q1).
- Kinetics of the antibody response:
- If the antibody response is a “long-term marker” (i.e., individuals who have ever been exposed to the pathogen/vaccine will have a response, regardless of how recently the exposure occurred), then frequent sampling may be less informative.
- If the antibody response is a “short-term marker” (i.e., only individuals who have recently been exposed to the pathogen/vaccine will have a response), then frequent sampling may be more informative.
- Note that an antibody response to a “long-term marker” will necessarily reflect recent exposure in children.
- Pathogen transmission dynamics: If the pathogen exhibits intra-annual seasonality, paired sampling at pre- and post-season will enable estimation of the attack rate that year. For newly emerged pathogens or pathogens exhibiting inter-annual differences in the force of infection, frequent sampling may be more informative.
- Control interventions and programmatic goals: If an intervention that will change pathogen exposure or seroprevalence will occur (e.g., a Supplemental Immunization Activity (SIA)), then sampling before and after will allow for evaluating the impact of the intervention. Conducting a “pre” serosurvey will be key for this.
- Feasibility: Leveraging existing platforms where samples are being collected periodically (e.g., DHS, HIV serosurveys) or continuously (e.g., residual specimens) will be less resource-intensive than de novo sample collection.
Potential Study Designs
- Leverage samples collected in another population-based survey (e.g., DHS, HIV serosurveys)
- Leverage residual samples being collected at inpatient or outpatient health facilities for other purposes (e.g., routine blood work)
- Collect samples from a predefined source population that may not be representative, but may be logistically more feasible (e.g., school-based surveys or at-home sampling)
Considerations
- The latter two study designs above are known as “convenience sampling”: using residual samples or samples from a predefined source population.
- Understanding how well a convenience sample reflects the target population will be important to properly interpret the results. It may be possible to reduce potential bias in convenience samples by incorporating additional meta-data into sample selection to better reflect the target population.
- For residual samples, an important sampling bias to consider is healthcare-seeking behavior as those providing the sample may not reflect the true underlying population. Having meta-data on the reason for the blood draw could be useful to understand this potential bias. Quantifying the bias will require comparing results from convenience sampling to results from a population-based serosurvey.
- Factors including potential biases, sample quality/storage, and ethical issues all need to be taken into account.
More information in module on residual specimens https://serosurveytools.org/residual-specimens/
This is an active area of inquiry and best practices are currently being developed. A common approach is to select one or multiple priority pathogens of interest, and power the serosurvey to estimate either an overall seroprevalence (or other epidemiologic quantity such as the force of infection) for that pathogen(s), or stratified by some covariate (e.g., age or a programmatically relevant spatial unit such as district). When considering multiple priority pathogens, choosing a strategy that optimizes the precision or relative margin of error around target estimates for all pathogens is preferable. If estimated seroprevalence is truly unknown, 50% seroprevalence could be used to provide the largest sample size estimates.
More information on sample size calculations available World Health Organization Vaccination Coverage Cluster Surveys: Reference Manual.
Table 2. Recommended minimal and additional variables for a multipathogen serosurvey and reasons for inclusion
| Variable | Reason |
|---|---|
| Date of specimen collection | Depending on how long it takes to conduct the serosurvey, calendar date may be associated with seroprevalence; e.g., for a recently emerged pathogen |
| Age | Age is often — but not always — associated with seroprevalence; e.g., when age is a proxy of cumulative exposure |
| Sex | The magnitude of antibody responses sometimes — but not always — varies by sex |
| Geographic indicator (such as household GPS) | Geography is often — but not always — associated with exposure |
| Variable | Reason |
|---|---|
| Vaccination status | This information will help interpret serostatus data for vaccine-preventable diseases |
| HIV status | Antibody responses may vary by individuals’ HIV status |
There may be other specific variables of interest depending on the serosurvey objectives, such malaria bednet usage if malaria program evaluation is the goal.
Resources